Nurses at Oklahoma State Hospital Who Apparently Contributed to the Deaths of 16 Babies
Infant bloodshed (the death of an babe within the first yr of life) is a widely-reported indicator of population health. This nautical chart drove highlights key infant mortality trends and demographic variation inside the United States and besides explores baby mortality rates in the U.S. compared to countries that are similarly wealthy and sizable (based on Gross domestic product and Gdp per capita).
Overall, the U.S. and comparable countries have seen a subtract in infant bloodshed rates in recent years, only the U.S. has been slower to improve its consistently higher average rate of infant deaths, and significant disparities exist inside the U.S. Although these gaps are not very clearly understood (in part due to express cross-national comparability and availability of data), we consider available data and recent enquiry to highlight some of the ameliorate-understood factors contributing to the U.S.'s relatively high rates of infant death.
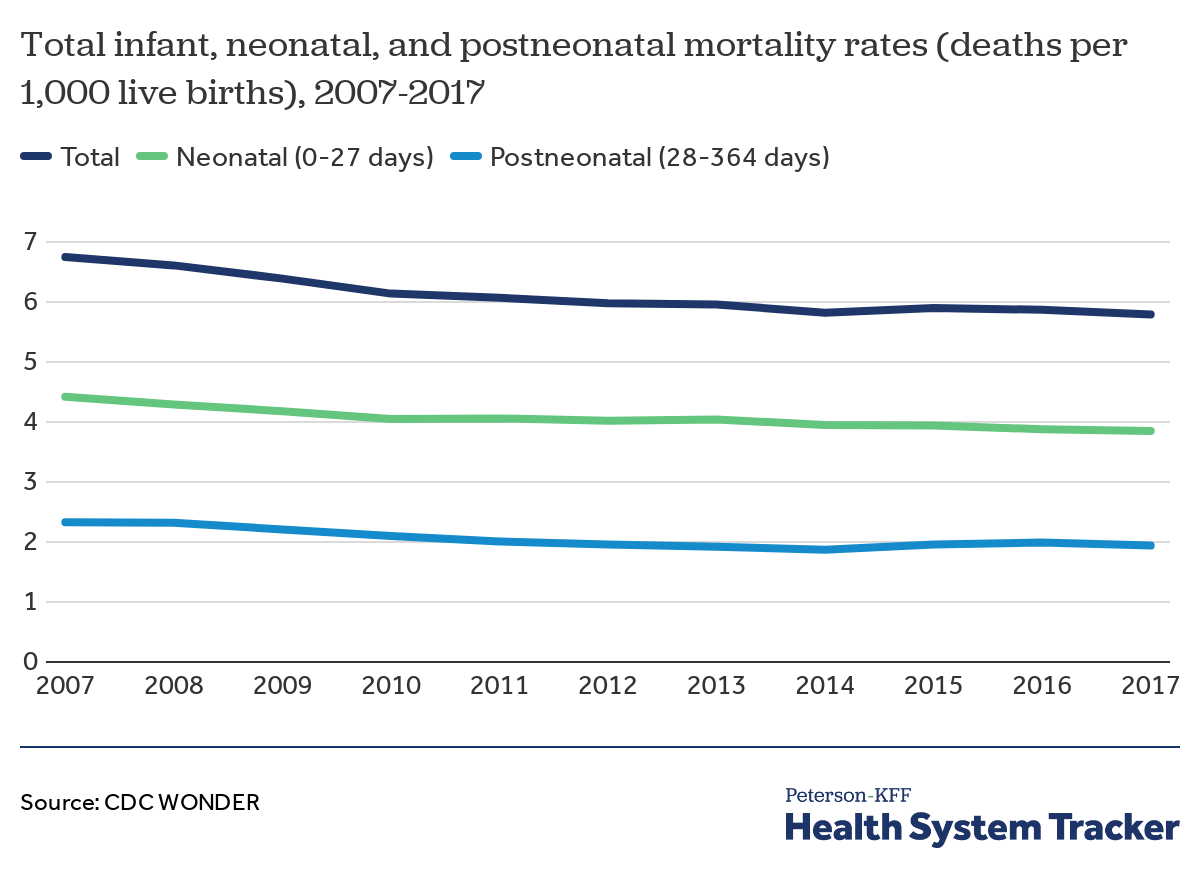
The U.S. infant mortality rate has improved over time
Over the past decade, the United States has seen reduced baby mortality. From 2007 to 2017, the U.S. infant mortality rate dropped by xiv percent (from 6.75 to 5.79 baby deaths per 1,000 alive births). Amid infant deaths, neonatal deaths are those which occur upwardly to 27 days later nascency, whereas postneonatal deaths are those occurring when the infant is 28 to 364 days of age. While both neonatal and postneonatal death rates accept declined (by xiii and 17 percent from 2007 to 2017, respectively), the larger share of infant deaths has consistently been neonatal deaths.
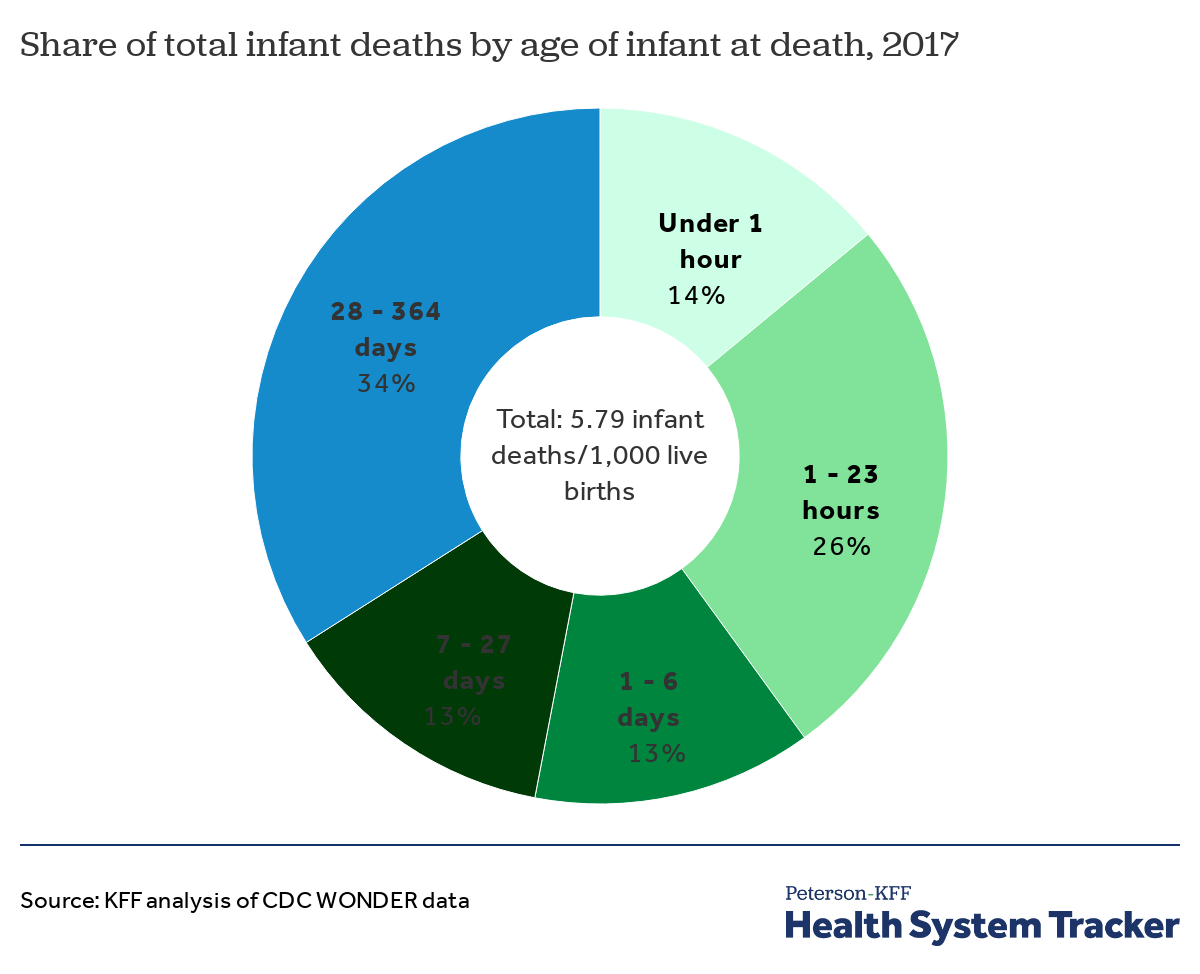
Two thirds of infant deaths in the U.Due south. occur within a calendar month after birth
While the majority of infant deaths in the U.S. occur less than 28 days after birth (the neonatal period), a substantial share occur 28 to 364 days after birth (the postneonatal menstruum). In 2017, 66 per centum of babe deaths occurred in the neonatal catamenia, and 40 pct of all infant deaths occurred specifically within the first 24 hours of birth. About a tertiary of infant deaths (34 percent) occurred in the postneonatal period.
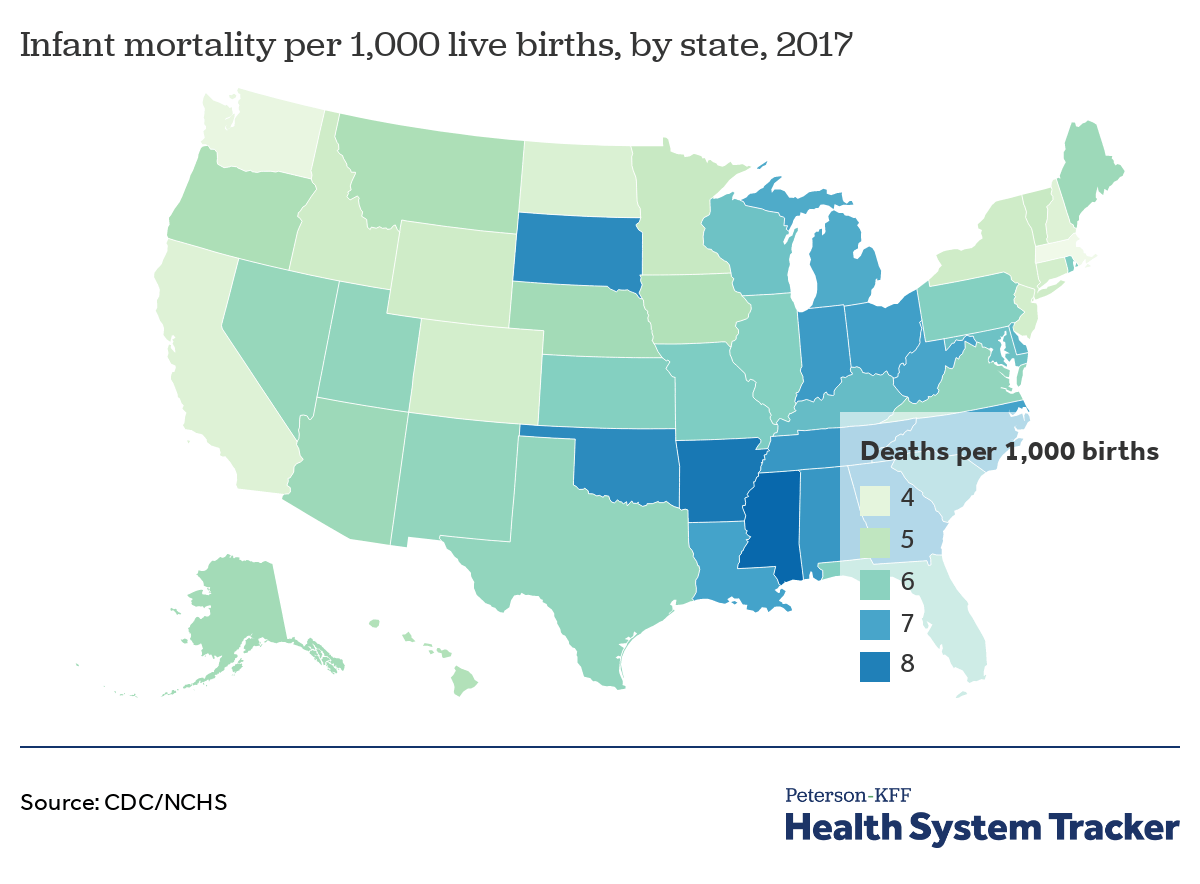
Infant mortality rates are relatively high in southern states
The U.South.'southward overall baby mortality rate is 5.79 deaths per one,000 alive births, but baby mortality rates vary from state to state, with a concentration of loftier rates in the South and parts of the Midwest. At the state level, babe mortality ranges from a low of 3.66 deaths per 1,000 live births in Massachusetts to a high of 8.73 in Mississippi. According to the National Center for Wellness Statistics, 11 states have infant mortality rates significantly lower than the national rate (CA, CO, CT, ID, MA, MN, NH, NJ, NY, ND, and WA), and xv states and the District of Columbia had significantly higher rates (AL, AR, GA, IN, KY, LA, Md, MI, MS, NC, OH, OK, SC, SD, and TN).
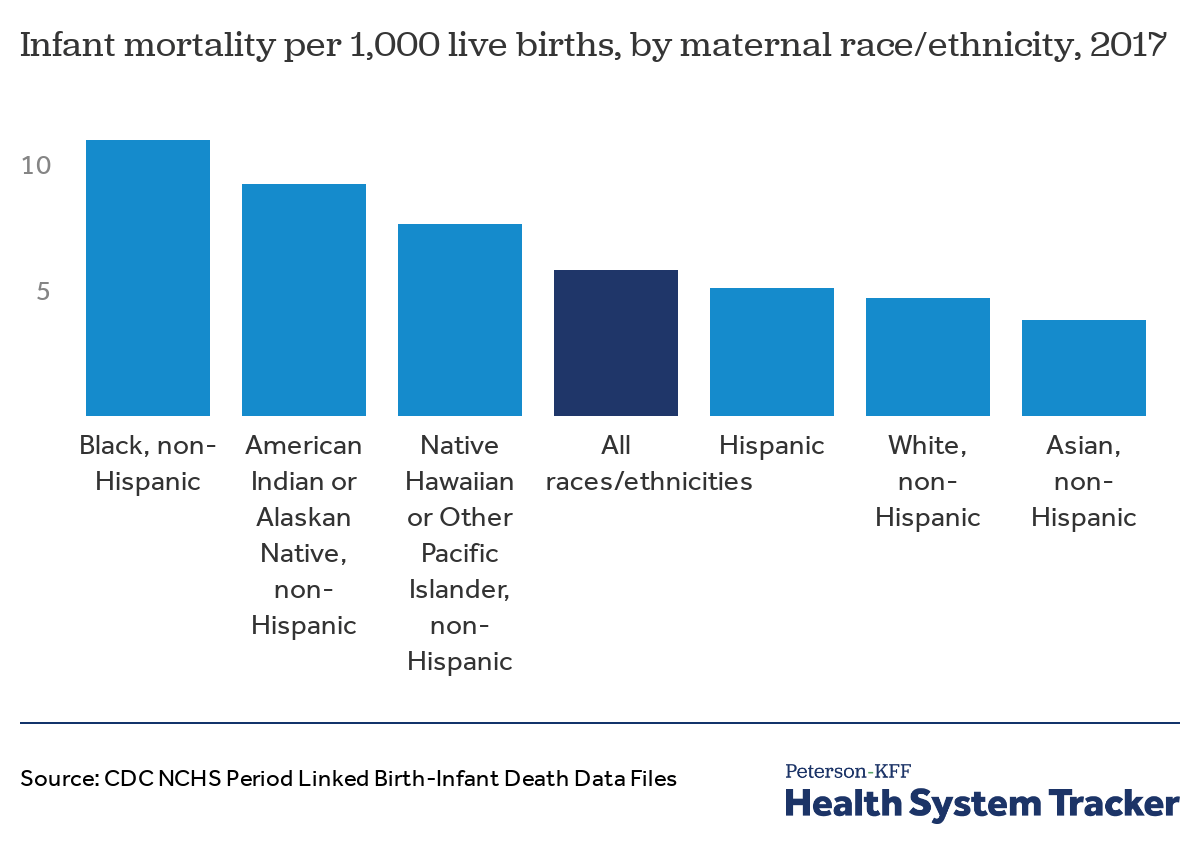
Mortality rates are higher than average among infants born to mothers who are Black, American Indian and Alaska Natives, and Pacific Islanders
At that place are significant racial disparities in infant mortality rates in the Usa. Not-Hispanic Blackness mothers experience the highest infant mortality rate among all racial and ethnic groups (10.97 baby deaths per one,000 alive births), as well as the highest rates of preterm nascency (delivery before 37 weeks of gestation) and low birth weight, both of which are leading causes of infant decease. Mothers who are American Indian or Alaska Native and Native Hawaiian or other Pacific Islander besides experience a higher than average infant mortality rate (9.21 and 7.64 deaths per 1,000 live births, respectively). The infant mortality rate among Hispanic mothers is similar to the national boilerplate (five.10 deaths per 1,000 live births), while rates amid White and Asian mothers are lower than average (4.7 and 3.8 deaths per ane,000 lives births, respectively).
Researchers have long considered a diverseness of complex factors in an effort to better sympathize racial disparities in infant mortality, including infant health; maternal demographics, health, and behavior; medical care before, during, and after birth; and dwelling and social environments before and after birth. Studies consistently indicate that socioeconomic disadvantage is linked to higher hazard of agin birth outcomes both in the U.S. and other highly industrialized countries, with substantial variation in how socioeconomic factors impact birth outcomes for different racial and ethnic groups.
Nevertheless, studies likewise increasingly note that socioeconomic disadvantages alone may not fully account for why Blackness mothers and their infants face such a disparity in agin maternal and babe health outcomes in the U.Due south., and researchers focusing on the substantial Black-White infant mortality gap have generally found that controlling for maternal background factors also does non fully explicate the disparity. Notably, recent research exploring U.Due south. maternal and infant health disparities discusses structural racism equally a primary take chances gene for African-American mothers and their infants, largely due to the complex stress it places on mothers throughout their life.
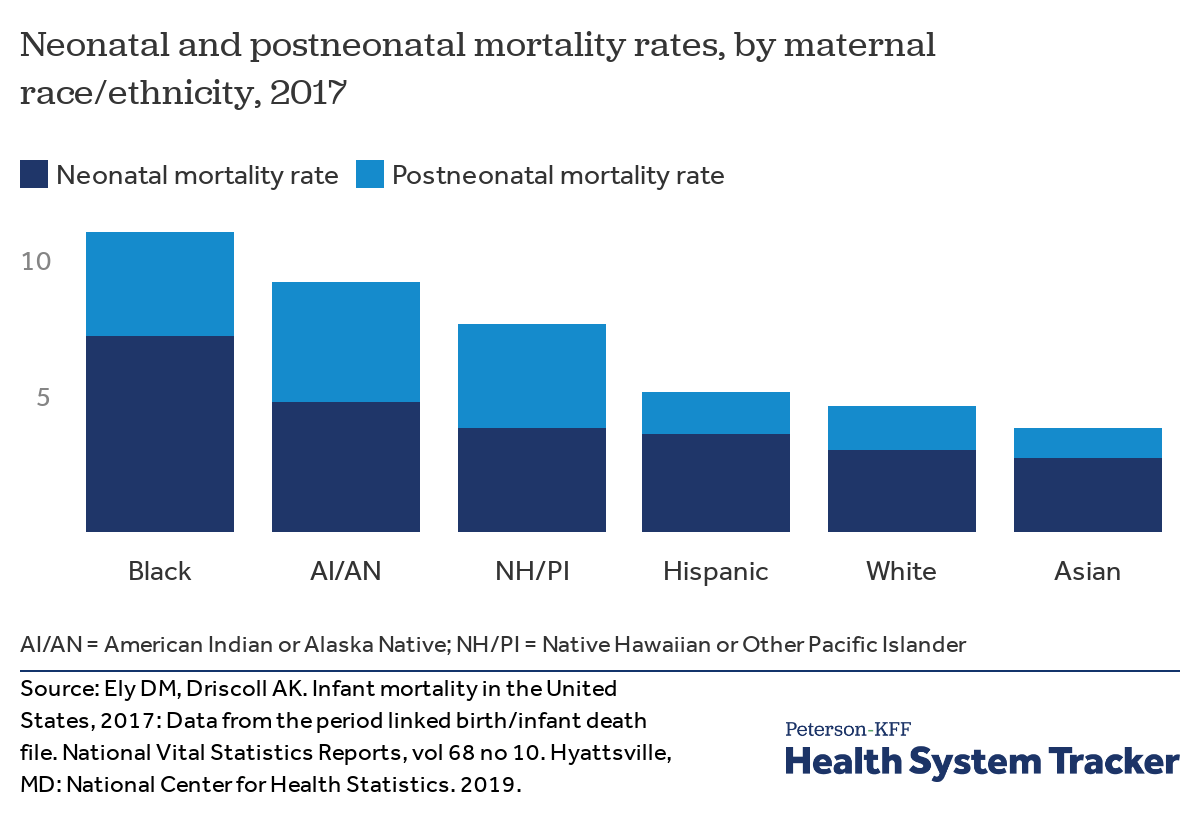
Neonatal mortality is highest amidst infants of Blackness mothers
Racial and indigenous disparities in infant mortality exist in both the neonatal and postneonatal menstruation. In 2017, neonatal mortality was highest amid infants of non-Hispanic Black mothers (vii.sixteen deaths per one,000 live births, compared to the national average of 3.85). Neonatal mortality was too in a higher place average amongst infants of non-Hispanic American Indian or Alaska Native mothers (4.77), was similar to the national boilerplate amid infants built-in to both non-Hispanic Pacific Islander (3.82) and Hispanic (3.56) mothers, and was below boilerplate amongst infants born to White (3.04) and Asian (2.71) mothers.
Postneonatal mortality was higher than the national average of ane.94 deaths per 1,000 live births for infants of non-Hispanic American Indian or Alaska Native mothers (4.41), non-Hispanic Blackness mothers (iii.82), and non-Hispanic Pacific Islander mothers (3.82).
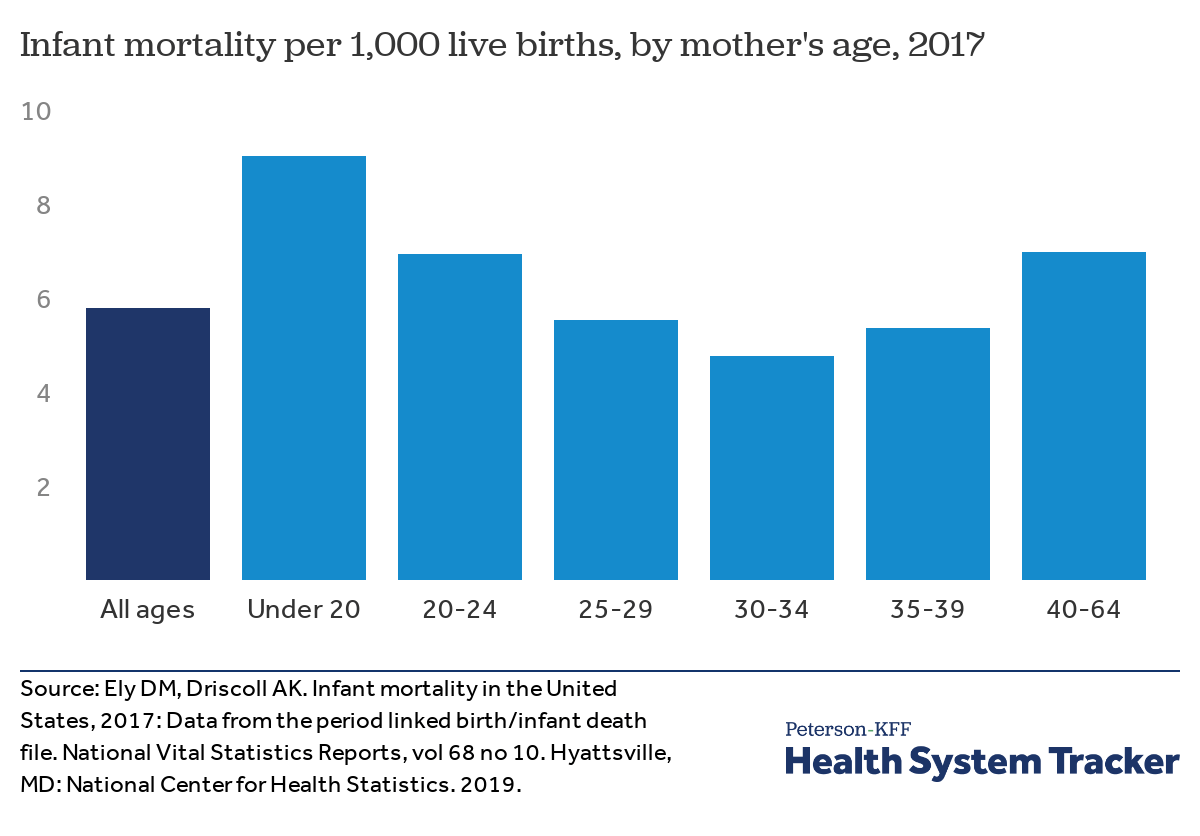
Infant mortality is highest among mothers nether age 20
Infant mortality varies considerably based on maternal age. The charge per unit of baby mortality is highest among mothers nether age xx (9.0 deaths per ane,000 live births) and lowest amongst mothers aged between 30-34 years old (4.eight deaths per 1,000 alive births).
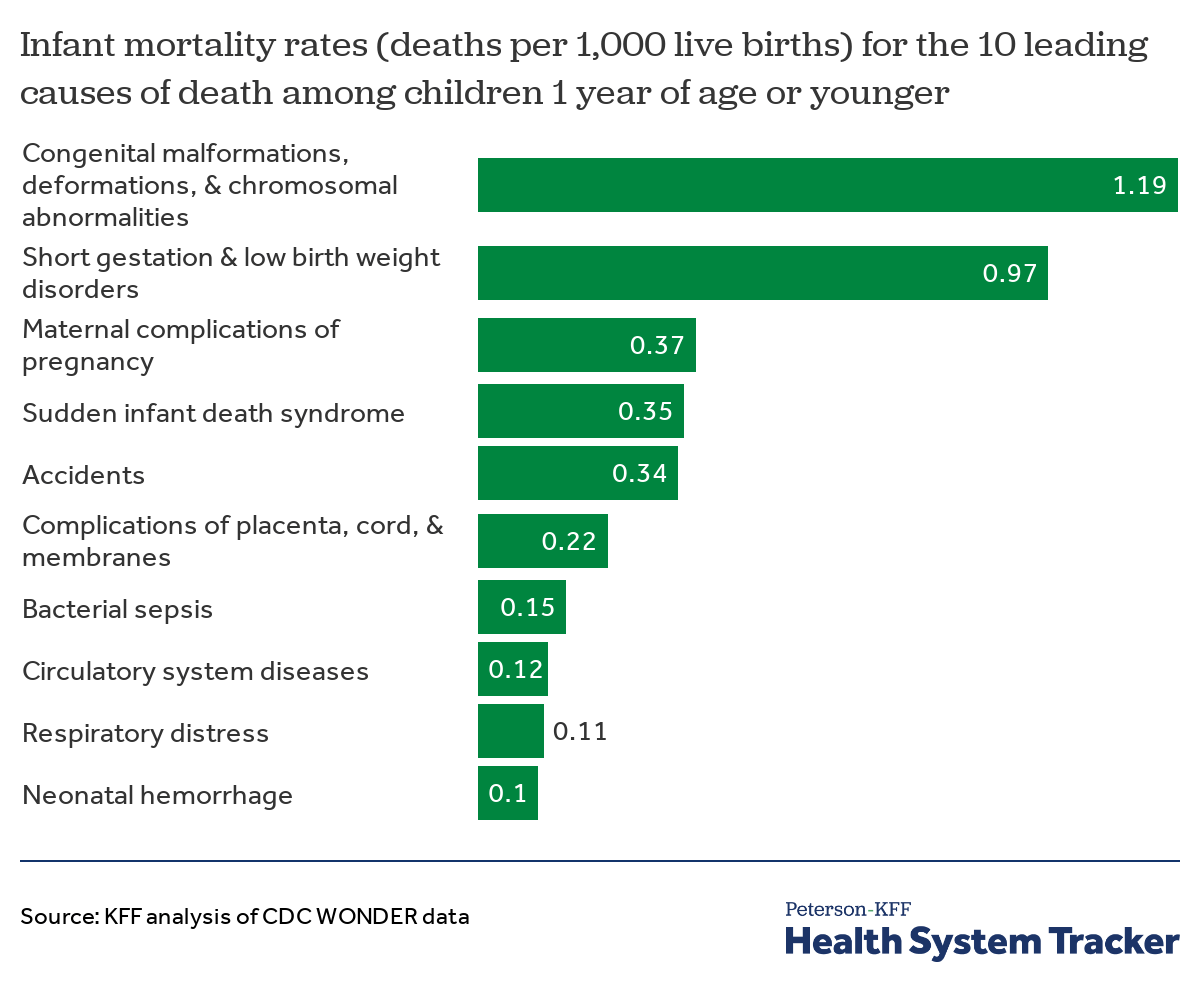
Congenital malformations are the most common cause of baby death in the U.S.
In 2017, 68 percent of all infant deaths in the U.Southward. were attributable to the x leading causes shown in the chart above. Built malformations were the underlying cause of 21 percentage of infant deaths, and short gestation and low nascence weight together accounted for 17 pct of infant deaths in the U.S.
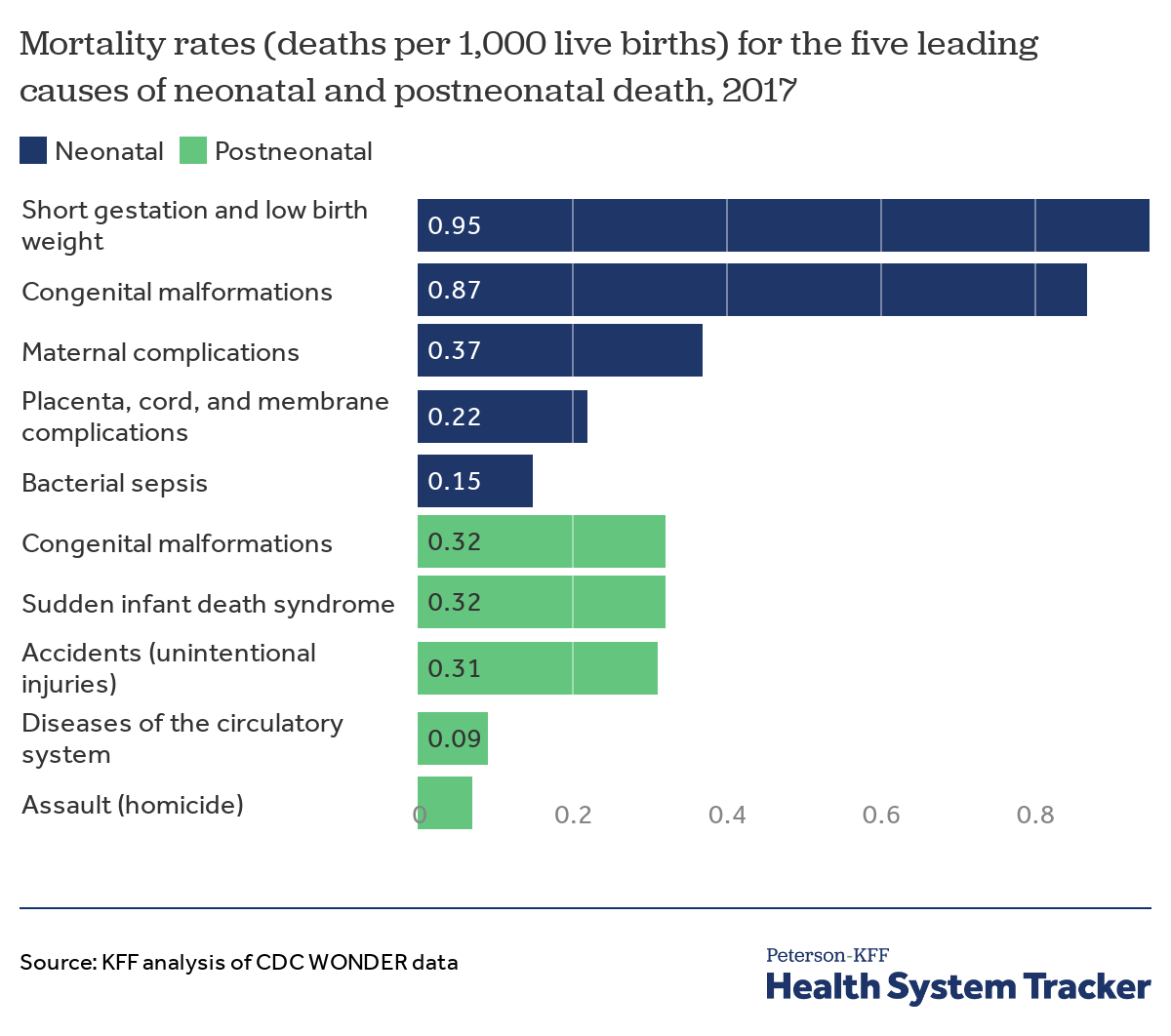
The leading causes of infant death in the U.S. vary before and after the infant is one month old
The chief causes of baby deaths vary by historic period of the infant at time of decease. Within the first month after birth, short gestation and low birth weight are together the leading cause of neonatal mortality (at a rate of 0.95 deaths per 1,000 live births), followed by built malformations (0.87 deaths per 1,000 live births) and maternal complications (0.37 deaths per ane,000 live births). In the postneonatal menstruation, the leading causes of death are built malformations complications (0.37 deaths per i,000 live births, Sudden Infant Expiry Syndrome (SIDS), and accidents (each accounting for well-nigh 0.iii deaths per 1,000 live births).
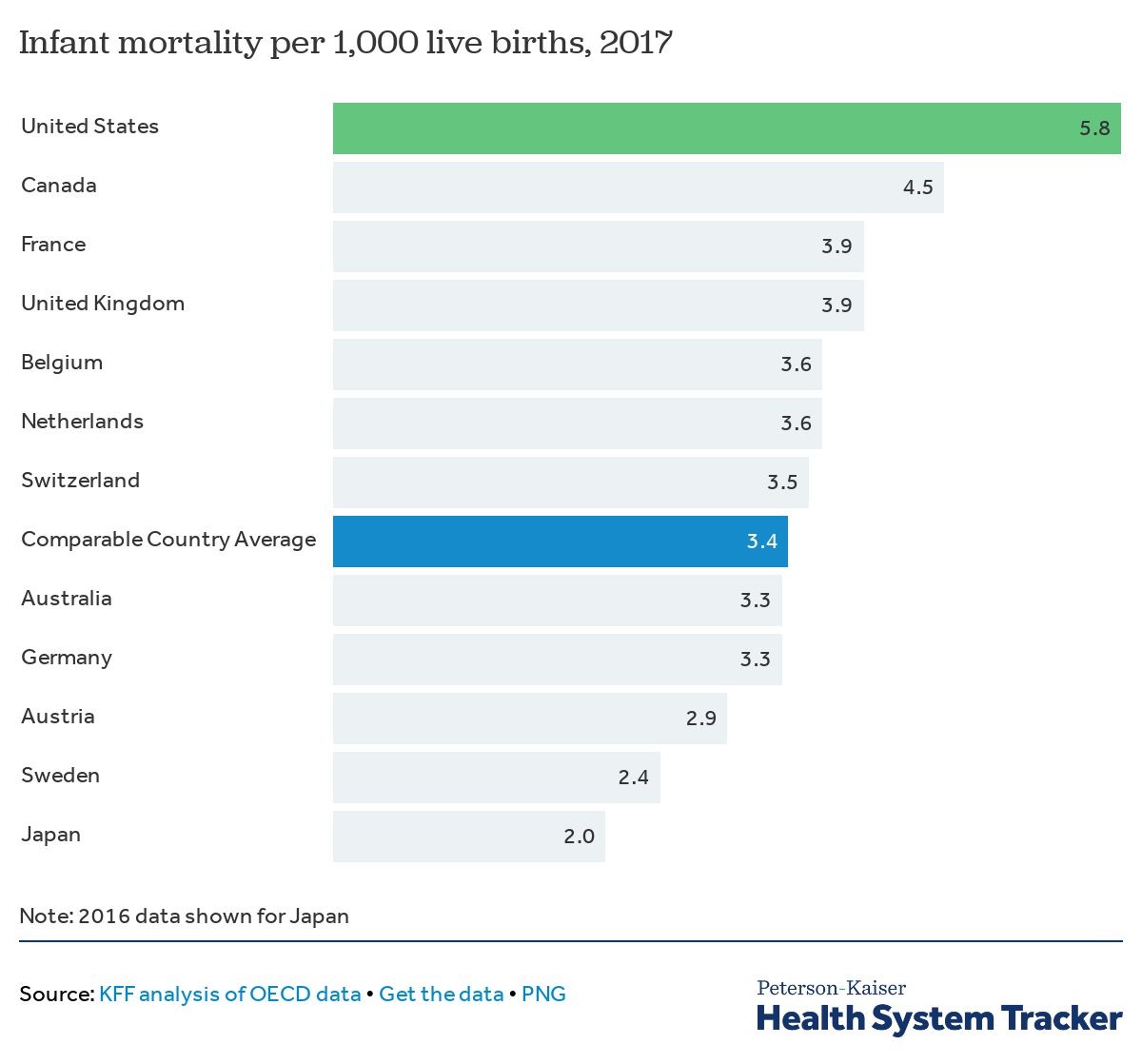
Infant mortality is college in the U.Southward. than in comparable countries
The U.Due south. infant mortality rate (5.8 deaths under 1 year of age per 1,000 live births) is 71 percent college than the comparable country average (iii.4 deaths). Research indicates socioeconomic inequality in the U.South. is likely a main contributor to its higher infant mortality, along with differential reporting methods. For case, a recent American Economic Journal study compared U.S. infant bloodshed to that of Republic of austria, Kingdom of belgium, Finland, and the United kingdom, concluding that data reporting differences may explicate up to about xxx percent of the gap betwixt the U.S. and these European countries. The written report finds that higher postneonatal bloodshed in the U.Due south. accounts for 30 to 65 per centum deviation and suggests socioeconomic weather condition among disadvantaged groups in the U.S. may account for most of its excess postneonatal mortality.
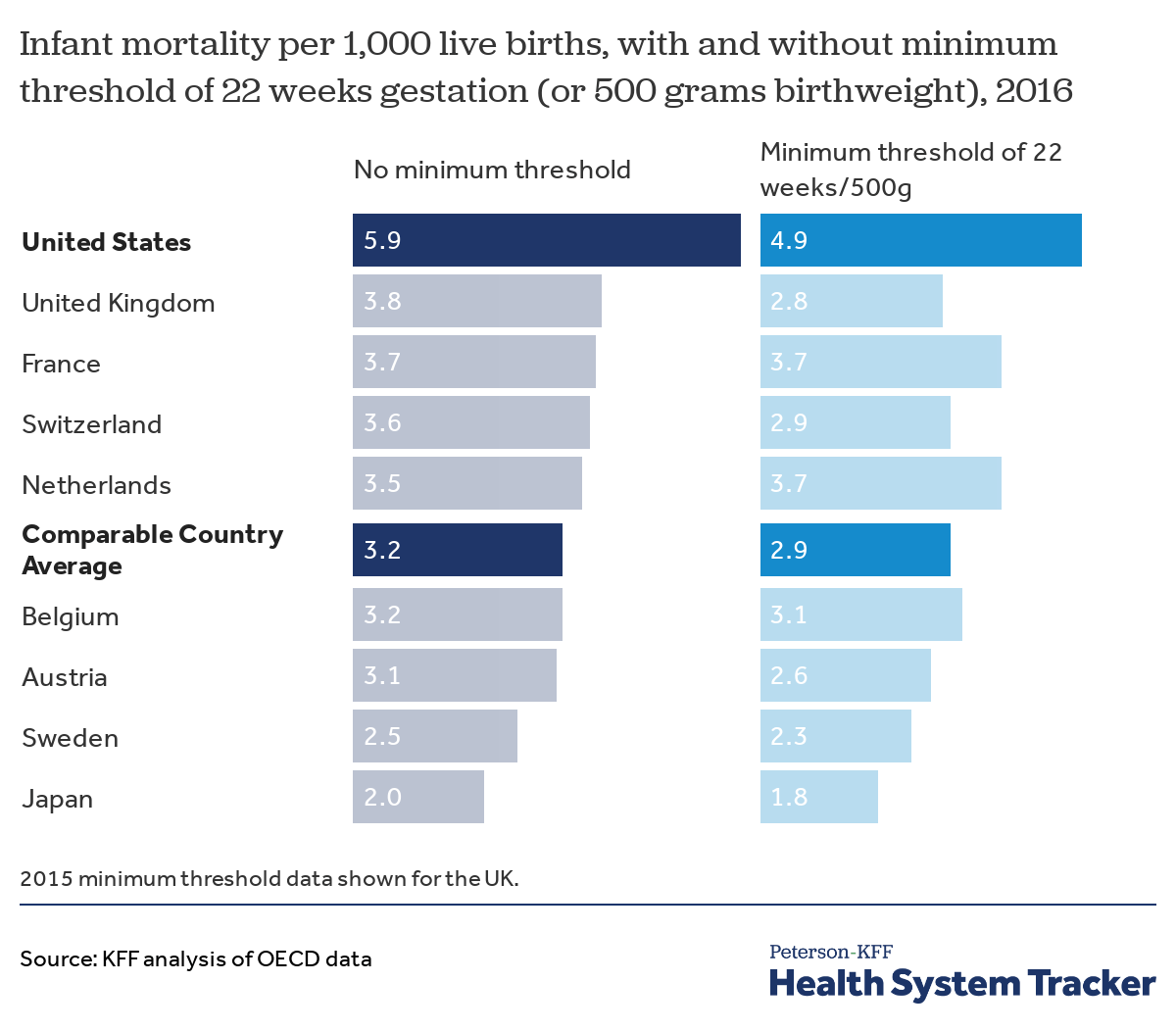
Bookkeeping for differential reporting methods, U.Due south. infant mortality remains higher than in comparable countries
When countries have different methods for reporting infant deaths, information technology is primarily a matter of how they written report deaths among infants with very low odds of survival. According to the OECD, the United states and Canada annals a higher proportion of deaths among infants weighing under 500g, which inflates the infant mortality rate of these countries relative to several European countries that count infant deaths as those with a minimum gestation age of 22 weeks or a nascency weight threshold of 500g.
Our assay of available OECD data for the U.S. and some similarly large and wealthy countries finds that when infant mortality is adjusted to include only those infant deaths that meet a minimum threshold of 22 weeks gestation or 500g in birth weight, the U.Southward. baby mortality rate is still higher than the average for those comparable countries with bachelor data (4.9 vs ii.ix deaths per 1,000 live births). Without adjusting for information differences, the U.S. infant mortality rate appears to be 84 percent college than the boilerplate for the same set of comparable countries. (Note that this comparison was limited to 2016 information and could not include data for Australia, Canada, and Germany, which are included in the previous chart's comparable country average for 2017.)
Infant bloodshed has declined more slowly in the U.S. than in comparable countries
While differences in information drove likely explain some of the variance in baby mortality rates by country, this should not impact the relative rates of change over fourth dimension, assuming information collection methods have not inverse considerably. From 2000 to 2017, the infant bloodshed rate in the U.S. barbarous from 6.9 to five.8 deaths per 1,000 live births, an improvement of 16 percent. Over the same period of time, the comparable land average improved by 26 pct, falling from 4.vi to 3.4 deaths per 1,000 alive births.
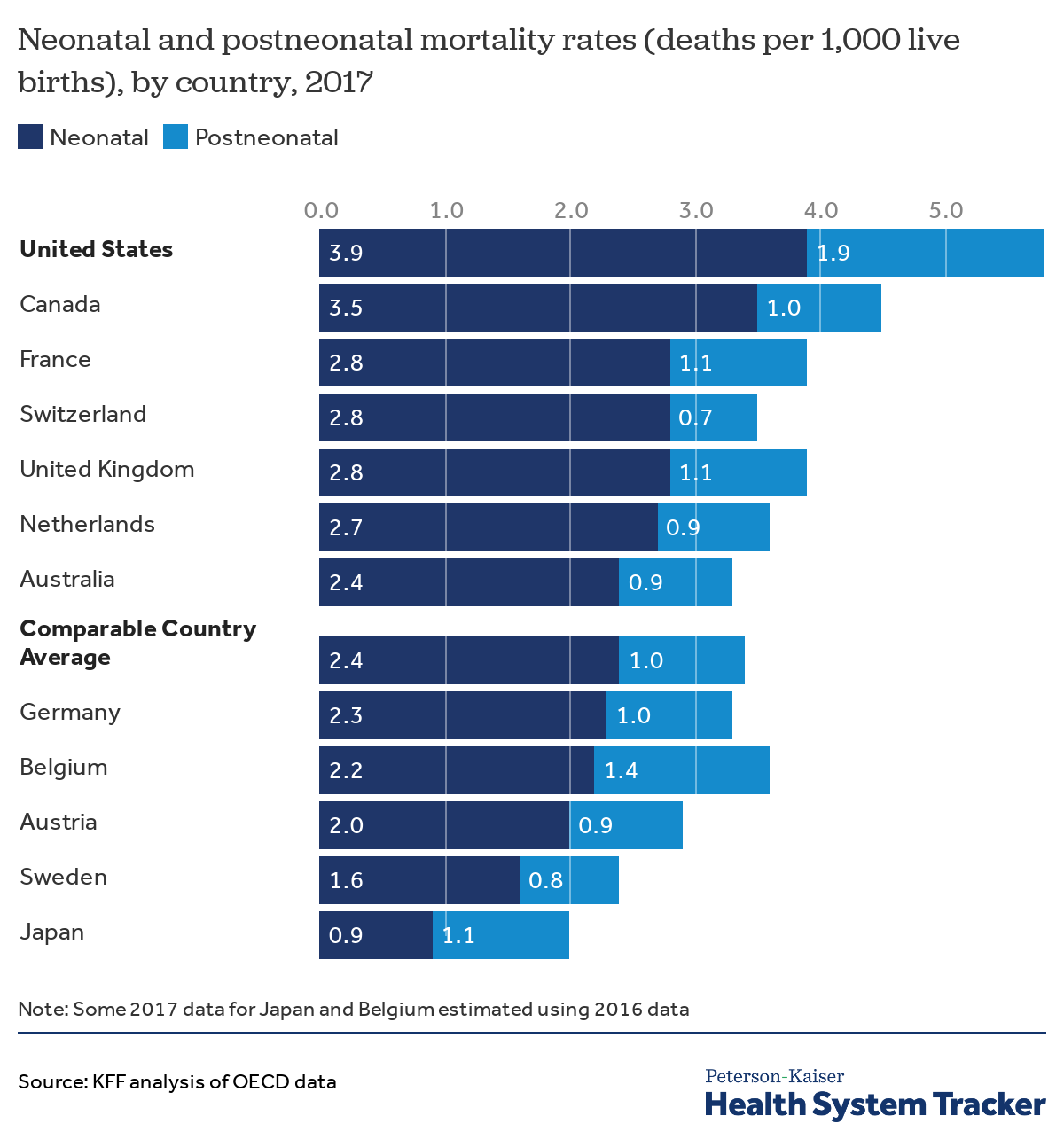
The infant mortality gap between the U.S. and comparable countries is more pronounced amongst postneonatal deaths
Relative to comparable countries on average, the U.S. has 63 pct more than neonatal deaths (iii.ix vs 2.iv deaths per 1,000 live births) and xc percentage more than postneonatal deaths (one.9 vs 1.0 deaths per 1,000 live births).
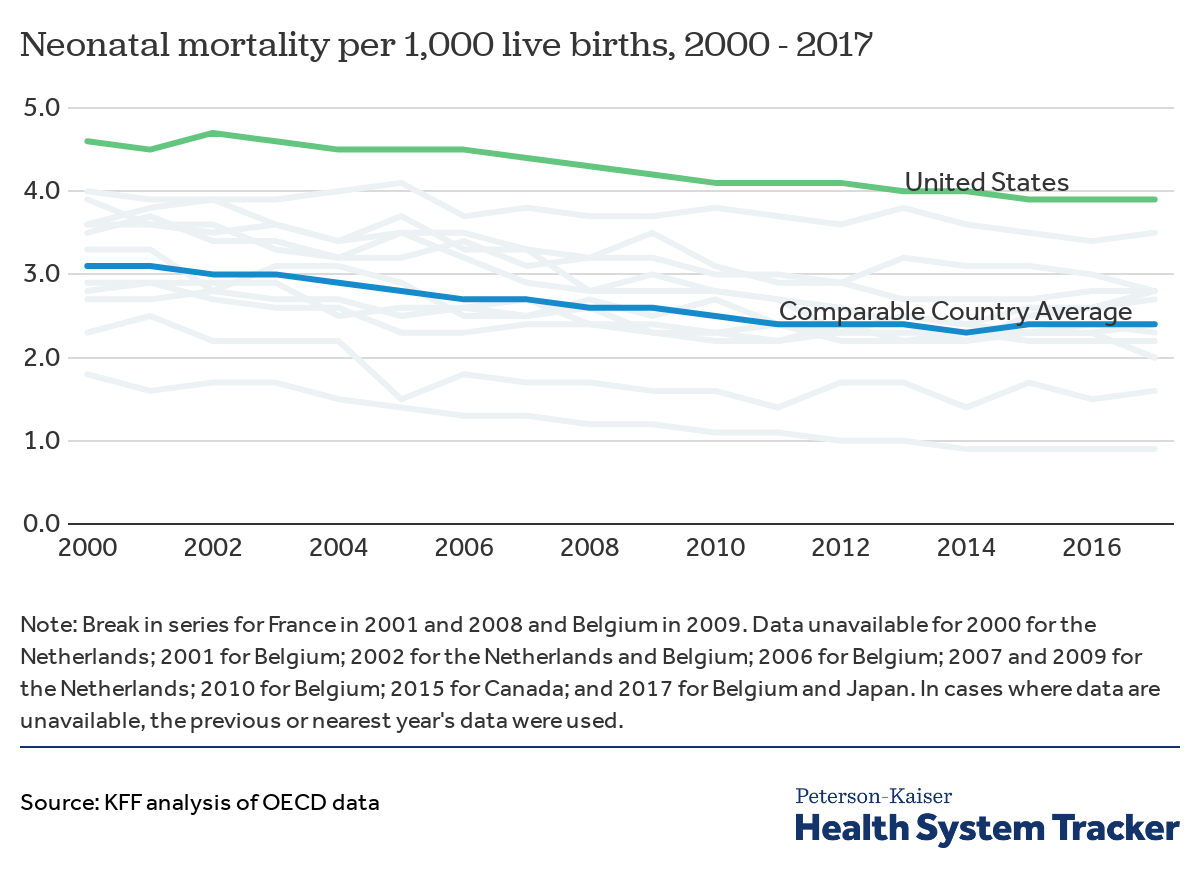
Neonatal bloodshed in the U.S. has improved more slowly than in comparable countries
From 2000 to 2017, neonatal deaths (deaths less than a month after birth) decreased by xv per centum in the U.S. and past 23 percent in comparable countries. Cross-national data reporting differences may explain some of the U.S.'s plainly lagging improvement.
Perinatal mortality in the U.S. is similar to comparable countries on average
Perinatal mortality rates, which reflect both early neonatal and some fetal deaths, are considered an indicator of the quality of antenatal and perinatal care. The U.S. perinatal mortality rate is like to the average rate across comparable countries (six.0 and 5.9 deaths per i,000 live births in 2016, respectively) and relatively lower than the charge per unit in some similarly wealthy countries. Information technology is not articulate if this variation reflects the quality of newborn intendance in the U.S., as international comparisons of perinatal mortality rates require conscientious scrutiny due to differences in registration practices.
The Peterson Center on Healthcare and KFF are partnering to monitor how well the U.S. healthcare organisation is performing in terms of quality and cost.
![]()
![]()
Source: https://www.healthsystemtracker.org/chart-collection/infant-mortality-u-s-compare-countries/


0 Response to "Nurses at Oklahoma State Hospital Who Apparently Contributed to the Deaths of 16 Babies"
Post a Comment